Campylobacter infections are a common occurrence in many parts of the world, and if you’ve ever fallen victim to this foodborne illness, you know just how miserable it can be. The Centers for Disease Control and Prevention (CDC) estimate that over 1 million people in the United States alone get campylobacter infection each year. But what causes these infections, and more importantly, how can you avoid getting one? In this article, we’ll delve into the world of campylobacter, discussing its causes, symptoms, diagnosis, treatment options, and most importantly, prevention strategies to reduce your risk of contracting this common illness.
Let’s explore together what it takes to stay safe from food poisoning. By understanding how campylobacter infections work, you can take proactive steps to protect yourself and your loved ones. Whether you’re a busy parent or an avid traveler, learning about food safety and handling practices is crucial in avoiding the discomfort of foodborne illnesses like campylobacter infection.
What is Campylobacter?
Let’s take a closer look at what campylobacter is: it’s one of the most common causes of food poisoning worldwide, affecting millions each year.
Definition and Prevalence
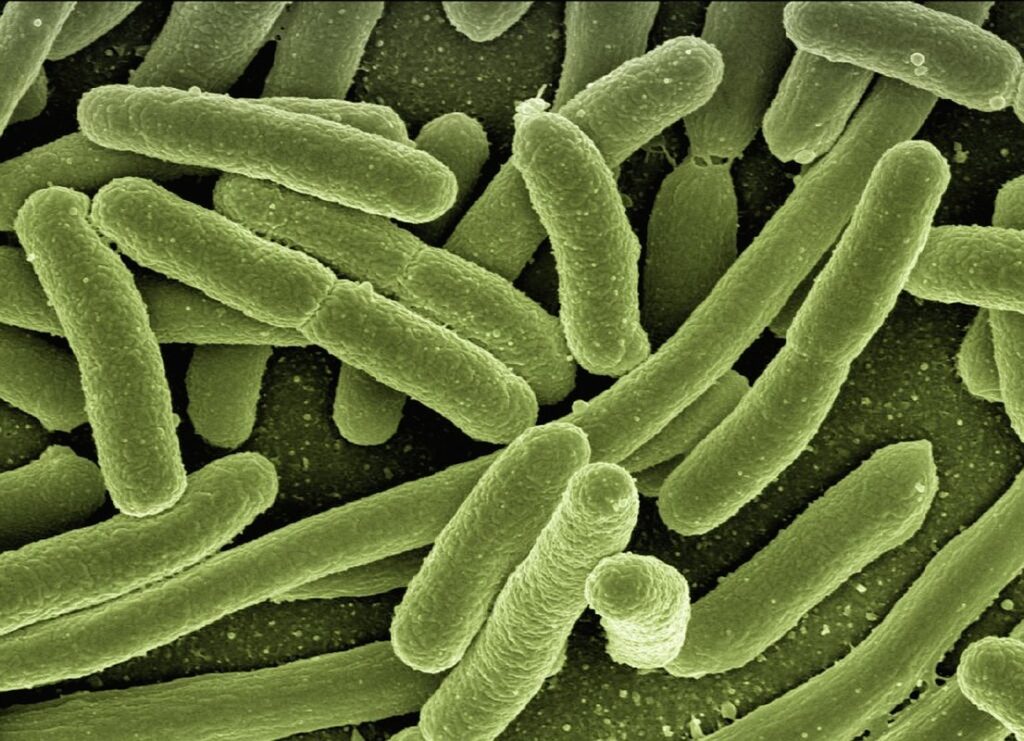
Campylobacter is a type of bacteria that causes one of the most common types of food poisoning worldwide. There are over 1,000 known species of Campylobacter, but the most prevalent ones are Campylobacter jejuni and C. coli. These two strains account for approximately 90% of all reported cases.
The prevalence rate of Campylobacter infection varies globally, with some countries experiencing significantly higher rates than others. According to the World Health Organization (WHO), an estimated one in ten people worldwide contract a Campylobacter infection each year. In the United States alone, it’s estimated that over 1 million cases occur annually.
In terms of regional prevalence, Europe has one of the highest rates of Campylobacter infections, with countries like Ireland and Denmark reporting some of the highest incidence rates globally. Understanding the types of Campylobacter and their worldwide prevalence is crucial for taking preventive measures to minimize the risk of infection. To stay safe, always handle raw poultry and meat properly, cook food thoroughly, and avoid cross-contamination in the kitchen. By being mindful of these simple practices, you can significantly reduce your chances of contracting a Campylobacter infection.
Symptoms and Complications
If you suspect that you have contracted campylobacter infection, be on the lookout for common symptoms such as diarrhea, fever, and abdominal cramps. These symptoms can range from mild to severe and usually start within two to five days after exposure to the bacteria.
In some cases, complications may arise if left untreated or under-treated. Gastroenteritis is a common complication that can lead to dehydration and electrolyte imbalances due to prolonged diarrhea and vomiting. If not managed properly, this condition can escalate into more severe forms of illness.
Guillain-Barré syndrome (GBS) is another rare but serious complication associated with campylobacter infection. This autoimmune disorder occurs when the immune system mistakenly attacks the nerves, causing muscle weakness and potentially leading to paralysis. GBS typically develops within weeks after infection, although in some cases it may take longer.
If you’re experiencing symptoms of gastroenteritis or suspect that you’ve contracted campylobacter infection, seek medical attention immediately to avoid potential complications like dehydration, electrolyte imbalances, and GBs. Your doctor can provide guidance on proper treatment and management.
Causes and Risk Factors
You may be wondering what can trigger a campylobacter infection, so let’s dive into the causes and risk factors that contribute to these outbreaks. Food and water contamination are common culprits in many cases.
Foodborne Transmission
Campylobacter is one of the most common causes of foodborne illness worldwide, and contaminated food products are often to blame. Poultry, meat, and unpasteurized dairy products are all potential carriers of Campylobacter bacteria.
When handling poultry, it’s essential to follow proper cooking techniques to ensure the meat reaches a safe internal temperature. According to the USDA, chicken breasts should be cooked to an internal temperature of at least 165°F (74°C) to kill any Campylobacter present. However, if you’re buying pre-cooked or processed meats, be aware that they may still harbor the bacteria.
In particular, unpasteurized dairy products like raw milk and soft cheeses are high-risk items for Campylobacter transmission. In 2018, a major outbreak of Campylobacter in the UK was linked to contaminated unpasteurized milk from a single farm. To avoid exposure through these products, opt for pasteurized alternatives or follow proper handling and storage procedures.
When shopping for meat or dairy, look for products that have been labeled as “pasteurized” or “hurdle technology” treated – these processes can significantly reduce the risk of contamination. Always store and handle these items safely, keeping raw meat separate from ready-to-eat foods to prevent cross-contamination.
Environmental and Personal Factors
In addition to food handling and preparation practices, there are several environmental and personal factors that can increase your risk of contracting a campylobacter infection. Poor hygiene is one such factor, as it can lead to the spread of bacteria through contaminated hands, surfaces, and utensils.
For instance, failing to wash your hands properly after using the bathroom or before handling food can transfer bacteria to other areas and make you more susceptible to infection. Similarly, touching raw meat, poultry, or seafood without washing your hands afterwards can also contribute to the risk of transmission.
Another significant environmental factor is contaminated water sources. If you drink or swim in water that has been contaminated with campylobacter bacteria, you may be at a higher risk of getting infected. This is particularly true for travelers who visit areas where water safety and sanitation practices are not up to par. To minimize your risk when traveling abroad, stick to bottled or filtered water and avoid consuming untreated lake or river water.
Traveling to areas with high campylobacter infection rates can also increase your risk of getting infected. Certain countries have higher rates of campylobacter infections due to factors such as poor sanitation, lack of access to clean water, or inadequate food handling practices. If you’re planning to travel to these areas, take extra precautions by washing your hands frequently, avoiding undercooked meat and poultry, and choosing reputable restaurants and food vendors.
Diagnosis and Treatment
Now that you know what campylobacter infection is, let’s discuss how doctors diagnose it and create an effective treatment plan to help you recover quickly.
Laboratory Tests
Diagnosing Campylobacter infections typically involves laboratory tests to identify the presence of the bacteria in stool samples. The most common method is a stool culture, where a sample is sent to a lab for growth and identification. However, this process can take up to 5-7 days, making it less ideal for timely diagnosis.
A more rapid approach is through Polymerase Chain Reaction (PCR) testing. This technique involves amplifying DNA sequences specific to Campylobacter to detect the presence of the bacteria. Results are typically available within 24 hours, making PCR a preferred method in many healthcare settings. Serology tests, which measure antibodies against Campylobacter, can also be used but are less commonly employed due to their lower specificity and sensitivity.
To ensure accurate diagnosis, it’s essential to collect and transport stool samples properly. This includes using sterile containers, keeping the sample refrigerated during transit, and storing it at 4°C if not tested immediately. Your healthcare provider will guide you through this process, which is critical for obtaining a reliable test result.
Antibiotic Therapy and Alternatives
If you’ve been diagnosed with campylobacter infection, your doctor may prescribe antibiotics to help manage symptoms and prevent complications. Currently, the most common antibiotic treatment for campylobacter infections is a macrolide (such as azithromycin) or a fluoroquinolone (such as ciprofloxacin). However, it’s essential to note that antibiotics only alleviate symptoms and don’t eliminate the infection entirely.
In recent years, researchers have explored alternative treatments to reduce antibiotic resistance. One promising area is probiotics, which can help restore gut flora balance and promote recovery. Studies suggest that probiotic supplements containing Lactobacillus acidophilus or Bifidobacterium bifidum can shorten illness duration and improve symptoms.
Herbal remedies like slippery elm and ginger have also shown potential in reducing inflammation and soothing digestive issues. However, more research is needed to confirm their efficacy and safety for campylobacter treatment. If you’re considering alternative approaches, consult with your healthcare provider before making any changes to your treatment plan.
Keep in mind that antibiotics can still be necessary for severe cases or those with underlying health conditions. Always follow your doctor’s guidance and complete the full course of prescribed medication to ensure optimal recovery.
Prevention and Control Measures
To minimize your risk of getting campylobacter infection, it’s crucial to understand how to prevent and control its spread. Here are some practical tips to help you stay safe.
Safe Food Handling Practices
When handling raw meat to prevent campylobacter infection, proper food safety techniques are crucial. Always wash your hands thoroughly with soap and warm water before and after handling raw meat, poultry, or seafood. This simple step can significantly reduce the risk of contamination.
Raw meat should be stored in sealed containers at the bottom of the refrigerator to prevent juices from dripping onto other foods. When transporting raw meat, use a separate cooler bag to keep it chilled and prevent cross-contamination with other food items. Before cooking, make sure raw meat is frozen according to package instructions or cooked immediately after thawing.
When preparing raw meat for cooking, always pat dry the surface with paper towels to remove excess moisture. This helps prevent bacterial growth during cooking. Use separate cutting boards, plates, and utensils for raw meat and ready-to-eat foods to avoid cross-contamination.
Remember to cook raw meat to the recommended internal temperature: 165°F (74°C) for ground meats, 145°F (63°C) for whole cuts of meat, and 145°F (63°C) for poultry. Use a food thermometer to ensure accurate temperatures.
Personal Hygiene and Environmental Cleaning
When it comes to preventing campylobacter infection, good personal hygiene and environmental cleaning practices are crucial. One of the most effective ways to reduce your risk is through handwashing. This simple yet essential habit should be practiced regularly throughout the day, especially after using the bathroom, before handling food, and after touching animals or their waste.
To wash your hands effectively, use soap and water for at least 20 seconds. Make sure to scrub all surfaces of your hands, including between fingers, under nails, and wrists. Rubbing your hands together is also essential in helping to dislodge any bacteria.
In addition to handwashing, environmental cleaning is also vital in preventing campylobacter infection. This includes regularly sanitizing high-touch areas such as doorknobs, light switches, and countertops using a disinfectant spray or wipes. Always clean up after handling raw meat, poultry, or their juices by washing utensils, cutting boards, and any other surfaces that may have come into contact with these substances.
Remember to also properly dispose of animal waste, such as pet droppings, and keep your living areas tidy to minimize the risk of campylobacter infection. By incorporating good hygiene practices into your daily routine, you can significantly reduce your chances of getting infected.
Emerging Trends and Research
Recent studies have shed light on the link between campylobacter infection and environmental factors, while others are exploring novel treatments to combat this bacterial illness.
Antimicrobial Resistance
As we continue to explore emerging trends and research surrounding Campylobacter infections, it’s essential to address a pressing concern: antimicrobial resistance. The overuse and misuse of antibiotics have contributed significantly to the rise of antibiotic-resistant bacteria, making treatment more challenging than ever.
According to the World Health Organization (WHO), Campylobacter is one of the leading causes of antibiotic-resistant infections globally. In fact, studies suggest that up to 90% of Campylobacter isolates are resistant to at least one antibiotic. This resistance isn’t limited to a single region; it’s a widespread issue affecting both developed and developing countries.
So, what can be done? Researchers are working tirelessly to develop new antibiotics specifically targeting Campylobacter bacteria. These novel compounds aim to overcome the limitations of current antibiotics and offer hope in the fight against antimicrobial resistance. In addition, healthcare professionals are emphasizing the importance of responsible antibiotic use – using them only when necessary and for the right duration. By adopting these strategies, we can mitigate the impact of antibiotic resistance and ensure effective treatment options remain available for those affected by Campylobacter infections.
Vaccination Efforts and Development
Researchers are actively exploring vaccine development as a potential game-changer in preventing Campylobacter infections. According to a 2020 study published in the journal Vaccine, several promising candidates have shown encouraging results in animal models and early human trials. These vaccines aim to target specific surface proteins or toxins produced by the bacteria.
One such candidate, CBIR1, has demonstrated impressive efficacy in reducing colonization rates by up to 90% in mice. Another vaccine, developed by a collaboration between academia and industry partners, has shown promising results in reducing symptoms in humans. While these findings are promising, it’s essential to note that further studies are needed to determine the long-term effectiveness of these vaccines.
As researchers continue to advance Campylobacter vaccine development, we can expect significant public health benefits. A successful vaccine could potentially reduce the estimated 1.3 million cases of Campylobacter infections in the US each year, as well as lower healthcare costs associated with these illnesses.
Frequently Asked Questions
Can I still be infected with Campylobacter even if my food looks and smells fine?
Yes, that’s correct. Campylobacter bacteria can survive on the surface of seemingly healthy foods, especially poultry and raw vegetables, without visible signs of spoilage. Always handle these foods safely, keeping them at a safe temperature to prevent cross-contamination.
How long after eating contaminated food will symptoms appear?
Symptoms of campylobacter infection typically take 2-5 days to develop after consuming contaminated food or water. However, in some cases, the incubation period can range from as short as 24 hours to up to a week or more. Keep track of your meals for at least 7 days to pinpoint when symptoms occur.
Are certain groups more susceptible to severe Campylobacter infection?
Yes, individuals with weakened immune systems, such as those undergoing chemotherapy, taking immunosuppressive medications, or living with chronic conditions like HIV/AIDS, are at a higher risk of developing severe campylobacter infections. Consult your healthcare provider about enhanced prevention strategies.
How can I clean my kitchen to prevent future Campylobacter outbreaks?
To maintain a safe kitchen environment, thoroughly clean and sanitize all surfaces with soap and water after each meal preparation. Pay special attention to areas around sinks, refrigerators, and cooking utensils. Consider implementing a regular deep-cleaning schedule, especially during peak illness seasons.
Can I take any steps to reduce my risk of Campylobacter infection while traveling?
Yes, definitely! While traveling abroad or domestically, stick to reputable food sources, especially when consuming raw foods like salads or sashimi. Choose restaurants that have good hygiene practices and are popular among locals. Also, avoid drinking tap water if it’s not known to be safe in the area you’re visiting.
