Are you aware that Salmonella Enteritidis is one of the most common causes of food poisoning in the world? This type of bacteria can contaminate eggs, meat, and other foods, putting millions of people at risk every year. If you’re like many others, you might be wondering what causes Salmonella Enteritidis infections, how to identify the symptoms, and most importantly, how to prevent them from happening in the first place.
As we delve into the world of foodborne pathogens, it’s essential to understand that Salmonella Enteritidis outbreaks can have serious consequences. In this article, we’ll explore the causes, symptoms, and prevention methods for this bacteria, as well as expert advice on handling outbreaks, diagnosis, and treatment options. By the end of this guide, you’ll be equipped with the knowledge to keep yourself and your loved ones safe from this potentially deadly pathogen.
What is Salmonella Enteritidis?
Salmonella Enteritidis is a type of bacteria that’s commonly found in poultry, and understanding its basics is crucial to protecting yourself from infection. Let’s break down what makes this particular strain so concerning.
Definition and Classification
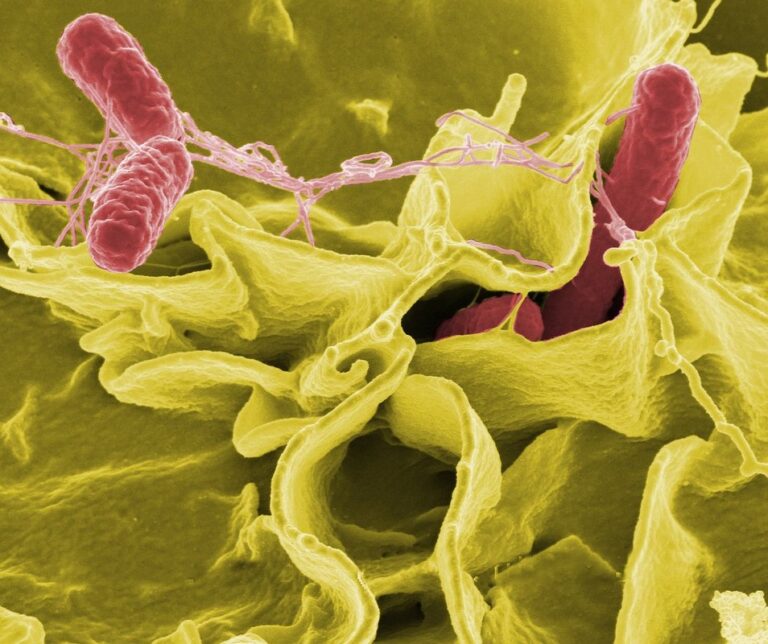
Salmonella Enteritidis (S. Enteritidis) is a specific strain of bacteria that falls under the Salmonella genus. It’s one of the most common types of Salmonella species responsible for foodborne illnesses worldwide. S. Enteritidis is classified as a Gram-negative, rod-shaped bacterium, and it’s often isolated from poultry products, particularly eggs.
To put its classification into perspective, there are over 2,500 known serovars of Salmonella, but only about 30 are commonly associated with human illness. Within this group, S. Enteritidis is one of the most significant causes of outbreaks in recent years. Unlike other Salmonella species like S. Typhimurium and S. Infantis, which are also prevalent in poultry, S. Enteritidis has a unique ability to adhere to and penetrate the egg yolk, making it particularly virulent.
This distinction makes understanding S. Enteritidis essential for proper food handling, storage, and preparation practices. Regular testing of eggs, strict hygiene measures, and thorough cooking can significantly reduce the risk of contracting this type of salmonella infection. When consuming poultry products, it’s crucial to prioritize safe food handling and be aware of the specific threats posed by S. Enteritidis.
History of S. Enteritidis Outbreaks
Salmonella Enteritidis (S. Enteritidis) has been responsible for numerous significant outbreaks and epidemics worldwide, causing substantial harm to public health. One of the most notable events was the 1984-1985 S. Enteritidis outbreak in England, where over 1,000 cases were reported, with many linked to contaminated eggs.
In the United States, a major outbreak occurred in 1990, resulting in 79 deaths and more than 8,500 illnesses attributed to S. Enteritidis-contaminated eggs from a single farm. This incident led to changes in egg production regulations and increased awareness about the risk of S. Enteritidis.
In recent years, large-scale outbreaks have been reported globally, including one in China in 2005 that affected over 14,000 people. These events highlight the importance of robust food safety measures, proper handling and storage practices, and continued research into prevention methods.
The recurring nature of these outbreaks underscores the need for vigilance and cooperation among governments, industry stakeholders, and consumers to prevent future occurrences.
Causes and Risk Factors
To better understand how you can contract Salmonella Enteritidis, let’s explore some of its most common causes and risk factors.
Contamination Sources
S. Enteritidis contamination can come from various sources, but some are more common than others. Poultry is one of the primary carriers of this bacteria, particularly chicken and turkey. According to the Centers for Disease Control and Prevention (CDC), poultry products such as raw ground poultry, deli meats, and even cooked poultry can be contaminated with S. Enteritidis.
Eggs are another significant source of contamination, especially if they come from infected hens. In fact, most S. Enteritidis outbreaks in the United States have been linked to eggs or egg products. To minimize the risk, it’s essential to handle and store eggs properly: keep them refrigerated at a temperature below 40°F (4°C), wash hands thoroughly before and after handling, and avoid consuming raw or undercooked eggs.
Meat, particularly chicken and beef, can also harbor S. Enteritidis bacteria, especially if not cooked to the recommended internal temperature of at least 165°F (74°C). Unpasteurized dairy products, like milk and cheese, are another potential source of contamination. When buying unpasteurized dairy products, check for certification from reputable organizations that ensure proper production practices.
In general, it’s crucial to handle and store all food products safely, especially those mentioned above. Regularly wash hands, clean kitchen surfaces, and cook food to the recommended temperature to prevent S. Enteritidis contamination.
Person-to-Person Transmission
When it comes to person-to-person transmission of S. Enteritidis, it’s often more about the behavior and habits that put people at risk, rather than an inherent trait of the bacteria itself. In most cases, S. Enteritidis is spread through close contact with someone who has the infection, such as a family member or caregiver.
This can occur when an individual with Salmonella comes into direct contact with another person’s mouth, eyes, or other mucous membranes. For example, if you’re caring for a loved one who has Salmonella and you touch their face or kiss them without proper hygiene practices, you may unintentionally spread the bacteria to yourself.
Contaminated food handling is also a common pathway for transmission. If someone prepares food while infected with S. Enteritidis, they can unknowingly contaminate surfaces, utensils, and other foods that others will come into contact with. To prevent person-to-person transmission of Salmonella, it’s essential to maintain proper hygiene practices, including frequent handwashing with soap and water, especially after using the bathroom or before handling food.
When in close proximity to someone who has been diagnosed with S. Enteritidis, take extra precautions: wash your hands regularly, avoid sharing utensils or personal items, and don’t kiss or engage in close physical contact until they’ve completed their treatment and been cleared by a healthcare professional.
Symptoms and Complications
If you suspect you have a salmonella infection, it’s essential to be aware of the common symptoms that may arise. We’ll break down what to expect if you contract Salmonella Enteritidis.
Common Symptoms in Humans
If you’ve contracted S. Enteritidis, you’re likely to experience a range of uncomfortable symptoms that can disrupt your daily life. The most common gastrointestinal issues associated with this infection are diarrhea and abdominal cramps, which can be quite severe in some cases.
Diarrhea is often the first symptom to appear, typically within 12-72 hours after exposure to contaminated food or water. In many instances, it’s accompanied by bloody stools, which can be a sign of inflammation in the intestines. Abdominal cramps are usually persistent and may radiate to other areas, making bowel movements even more painful.
Fever is another symptom that often accompanies these gastrointestinal issues, with temperatures typically ranging from 101°F to 103°F (38.3°C to 39.4°C). Some people may also experience nausea, vomiting, or headaches, while others might experience fatigue and chills as their body fights off the infection. Keep in mind that not everyone will exhibit all of these symptoms simultaneously, but they’re all common indicators of S. Enteritidis infection.
High-Risk Groups and Complications
When it comes to S. Enteritidis infections, some groups are more susceptible to severe complications than others. This is due to various factors such as age, underlying health conditions, and weakened immune systems.
The elderly, for instance, may have a harder time fighting off the infection due to declining physical function and reduced immunity with age. According to the Centers for Disease Control and Prevention (CDC), people over 65 years old are at higher risk of developing severe illnesses from S. Enteritidis. Their weakened immune response can lead to more serious complications such as sepsis, organ failure, or even death.
Young children under five also fall into a high-risk category due to their immature immune systems and lack of hygiene practices. This age group may not be able to fully express symptoms like diarrhea and vomiting, making it difficult for parents to recognize the severity of the infection.
Individuals with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy, are also more prone to severe complications from S. Enteritidis infections. These individuals require extra precautions when handling food and observing proper hygiene practices to minimize their risk.
Diagnosis and Treatment
If you suspect you’ve contracted Salmonella Enteritidis, understanding the diagnosis and treatment process can help alleviate your concerns. We’ll guide you through how it’s typically identified and managed by healthcare professionals.
Laboratory Testing Methods
Accurate diagnosis of S. Enteritidis infections relies on laboratory testing methods that can identify the presence and characteristics of the bacteria. Culture is a traditional method used to isolate and grow S. Enteritidis from stool samples or other contaminated materials. However, this process can take several days to yield results.
Polymerase chain reaction (PCR) is a more rapid technique that amplifies specific DNA sequences of S. Enteritidis, allowing for faster diagnosis. PCR has become increasingly popular due to its high sensitivity and specificity, reducing the risk of false positives or negatives.
Serotyping involves identifying the specific antigenic properties of S. Enteritidis, helping healthcare professionals understand the strain’s potential severity and treatment options. This method is particularly useful in epidemiological investigations to track outbreaks and monitor disease spread.
In practice, laboratories may use a combination of these methods to confirm diagnosis. For instance, PCR might be used initially, followed by serotyping if the results are positive. By understanding the laboratory testing methods available for diagnosing S. Enteritidis infections, individuals can better navigate the diagnostic process and take informed steps towards treatment and prevention.
Antibiotic Therapy and Supportive Care
When treating an S. Enteritidis infection, it’s essential to focus on both antibiotic therapy and supportive care to manage symptoms and prevent complications.
Antibiotic therapy is often the primary treatment for S. Enteritidis infections, particularly in severe cases or those involving vulnerable populations such as the elderly, young children, or people with weakened immune systems. However, it’s crucial to note that antibiotics are not effective against all types of Salmonella, including S. Enteritidis. For most cases, supportive care is recommended.
Supportive care typically involves managing symptoms and preventing complications through hydration, rest, and a bland diet. This can include:
• Encouraging plenty of fluids to prevent dehydration
• Resting and avoiding strenuous activities until symptoms subside
• Eating small, frequent meals of easily digestible foods such as crackers, bananas, or applesauce
• Avoiding high-fiber foods, dairy products, and fatty or spicy foods that can exacerbate symptoms
In some cases, hospitalization may be necessary to manage severe dehydration, electrolyte imbalances, or other complications. If you suspect an S. Enteritidis infection, it’s essential to seek medical attention promptly to receive proper treatment and prevent long-term health consequences.
Prevention and Control Measures
To prevent Salmonella Enteritidis infections, it’s essential to take practical steps in your daily life and in food handling practices. This section will walk you through those key measures.
Food Safety Guidelines
When handling and preparing food to prevent S. Enteritidis contamination, it’s essential to follow proper guidelines. First and foremost, always choose eggs from reputable sources that have a good record of safety. Raw or undercooked eggs can pose a significant risk, so it’s crucial to cook them thoroughly before consumption.
To ensure your eggs are cooked properly, make sure they reach an internal temperature of at least 160°F (71°C). For example, when making omelets or scrambled eggs, use a food thermometer to check the temperature. When baking goods like cakes and cookies that contain raw eggs, it’s also vital to follow safe minimum internal temperatures.
Proper storage is another critical aspect of preventing S. Enteritidis contamination. Always store raw eggs in their original carton on the middle or bottom shelf of your refrigerator to prevent them from coming into contact with other foods. Cooked and ready-to-eat foods should be refrigerated at a temperature of 40°F (4°C) or below within two hours.
Finally, always wash your hands thoroughly before handling food, especially when preparing raw eggs. This simple step can significantly reduce the risk of cross-contamination.
Public Health Strategies
Public health officials play a critical role in controlling and preventing S. Enteritidis outbreaks through targeted surveillance, swift outbreak investigation, and informed education campaigns.
To get ahead of potential outbreaks, public health officials should conduct regular surveillance on poultry farms, processing plants, and retail stores. This involves monitoring for any signs of contamination, such as unusual illness clusters or positive laboratory results. For instance, in 2019, the CDC reported a significant increase in S. Enteritidis cases linked to chicken eggs from a single farm in California. Through proactive surveillance, public health officials identified the source and alerted the industry, preventing further outbreaks.
During an outbreak investigation, officials work quickly to identify the source, contain the spread, and implement control measures. This may involve recalling contaminated products, closing affected facilities, or advising consumers on safe food handling practices. A thorough investigation also helps officials understand how the outbreak occurred, allowing them to make targeted recommendations for prevention.
Education campaigns are essential in empowering consumers with knowledge on proper food handling and storage techniques. Public health officials can partner with farmers, processors, and retailers to disseminate key messages through various channels, such as social media, print ads, or community outreach programs. By raising awareness about S. Enteritidis risks and promoting safe practices, public health officials can significantly reduce the incidence of these outbreaks.
In addition to surveillance, outbreak investigation, and education campaigns, public health officials should also collaborate with industry partners to implement long-term solutions. This might involve establishing guidelines for proper egg washing and packing procedures or supporting research on improved detection methods.
Public health officials should also consider utilizing various data sources and tools to enhance their response efforts, such as:
* Integrating laboratory results into electronic surveillance systems
* Analyzing consumer reports of illness using mobile apps or online platforms
* Employing predictive modeling techniques to forecast potential outbreak hotspots
By employing these strategies in a coordinated and proactive manner, public health officials can effectively control and prevent S. Enteritidis outbreaks, ultimately protecting consumers and preserving the integrity of the food supply chain.
Global Outbreaks and Surveillance
As we explore the global impact of Salmonella Enteritidis, let’s take a closer look at how outbreaks are tracked and monitored in real-time, highlighting key international surveillance efforts. This helps us stay ahead of the bacteria.
International Collaboration and Reporting
The global spread of Salmonella Enteritidis (S. Enteritidis) necessitates international collaboration and surveillance efforts to detect, report, and control outbreaks effectively. Organizations like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) facilitate information exchange and coordination among countries through networks such as PulseNet.
PulseNet is a global network of public health laboratories that share data on foodborne disease outbreaks using whole-genome sequencing (WGS). This collaboration enables rapid identification of outbreak strains, facilitating timely response and control measures. For instance, in 2019, the CDC utilized PulseNet to track an S. Enteritidis outbreak linked to contaminated eggs across multiple states in the US.
International reporting is also crucial for identifying trends and understanding the global burden of S. Enteritidis infections. The WHO’s Global Foodborne Infections Network (GFN) promotes collaboration among countries to monitor and respond to foodborne outbreaks, including those caused by S. Enteritidis. By sharing data and best practices, countries can work together to reduce the incidence of S. Enteritidis infections worldwide.
To stay informed about global S. Enteritidis outbreaks, public health professionals can follow PulseNet’s online database and participate in international forums like the WHO’s GFN meetings. Additionally, researchers and policymakers can leverage international datasets and reports from organizations such as the CDC and WHO to inform evidence-based decision-making and control strategies.
Emerging Trends and Challenges
The emergence of antimicrobial resistance (AMR) is a pressing concern when it comes to S. Enteritidis infections. As bacteria adapt and evolve, our traditional treatments are becoming less effective, making AMR a significant challenge for public health authorities. In fact, according to the World Health Organization (WHO), AMR is one of the top 10 global health threats facing humanity.
In response, some countries have implemented new strategies to tackle AMR, such as restricting antibiotic use in agriculture and promoting antimicrobial stewardship programs in healthcare settings. These efforts are essential, but more needs to be done. Individuals can also play a role by following proper food handling and cooking practices, especially when it comes to poultry products.
Another emerging trend is the changing epidemiology of S. Enteritidis infections. As global trade and travel increase, we’re seeing new strains and serotypes emerge in different regions. This highlights the need for continued surveillance and collaboration among international health authorities to stay ahead of the curve.
Frequently Asked Questions
Can I get Salmonella Enteritidis from handling contaminated food or is it airborne?
Yes, you can get infected through direct contact with contaminated food, particularly raw eggs, poultry, and meat. However, proper hand hygiene and cleaning of surfaces can significantly reduce the risk. To minimize exposure, always wash your hands thoroughly after handling food, especially after being in contact with potentially contaminated items.
How long does it take to show symptoms after exposure to Salmonella Enteritidis?
The incubation period for Salmonella Enteritidis typically ranges from 6 hours to 6 days, with most people showing symptoms within 12-24 hours. Be cautious if you experience diarrhea, fever, or abdominal cramps shortly after consuming potentially contaminated food.
What are the essential steps I should take to prevent Salmonella Enteritidis infections in my household?
To keep your family safe from Salmonella Enteritidis, practice good hygiene habits: wash hands frequently with soap and water, especially before handling food. Cook poultry and eggs thoroughly until they reach an internal temperature of at least 165°F (74°C). Regularly clean and sanitize kitchen surfaces, utensils, and equipment.
Can antibiotics cure Salmonella Enteritidis infections?
No, antibiotics are not recommended for treating mild cases of Salmonella Enteritidis as they can sometimes make symptoms worse. In severe cases or when the infection leads to complications like blood poisoning, treatment typically involves supportive care and hydration rather than antibiotic therapy. Antibiotics should only be prescribed by a healthcare professional in specific circumstances.
How often do I need to check for laboratory-confirmed outbreaks of Salmonella Enteritidis in my area?
Regular updates on local outbreaks can help you stay informed about the risk levels in your community. Consult official health department websites or subscribe to their newsletters for timely information on foodborne illness outbreaks and prevention measures in your region.
