Campylobacter infections are more common than you think. In fact, this bacterial illness is one of the most frequently reported foodborne illnesses in many parts of the world. If you’ve ever had a bout of diarrhea, stomach cramps, and fever that seemed to come out of nowhere, you might have unknowingly contracted campylobacter. The good news is that with proper knowledge and precautions, you can protect yourself and your loved ones from this common bacterial illness.
In this article, we’ll take a closer look at the causes and symptoms of campylobacter infection, as well as the ways to diagnose and treat it. We’ll also explore effective prevention methods to keep you safe from this unwelcome visitor in the future. By learning more about campylobacter, you can better equip yourself to identify potential threats and take steps to stay healthy.
What is Campylobacter?
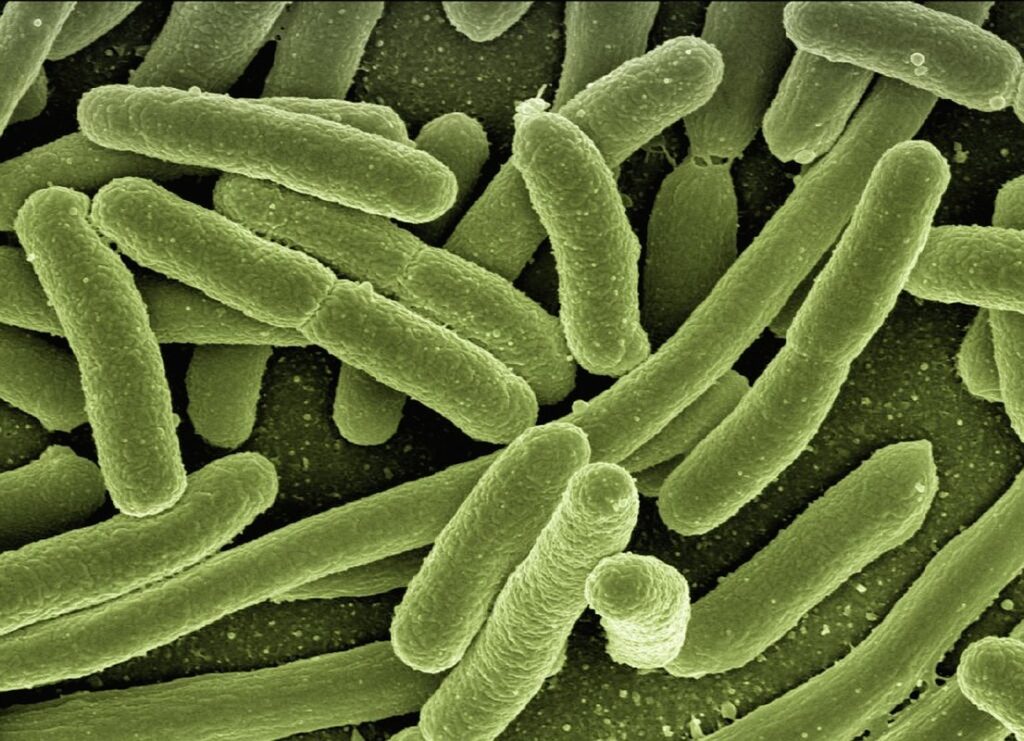
Let’s start by understanding what campylobacter is: a type of bacteria that can cause a highly contagious and potentially severe foodborne illness. We’ll break down its characteristics next.
Definition and Classification
Campylobacter is a type of bacterial species that causes one of the most common foodborne illnesses worldwide. To understand Campylobacter better, it’s essential to grasp its classification and characteristics.
As a member of the Epsilonproteobacteria group, Campylobacter belongs to the family Campylobacteraceae. This group comprises several species, with Campylobacter jejuni being the most prevalent cause of human infections, responsible for approximately 80% of all cases. Other notable species include Campylobacter coli and Campylobacter lari.
These bacteria are highly adaptable and can thrive in various environments, including water, soil, and animal intestines. They’re often transmitted to humans through contaminated food or water, with undercooked poultry being a common source of infection.
It’s worth noting that the classification of Campylobacter species is based on their biochemical properties, such as their ability to ferment certain sugars. This classification helps researchers understand the behavior and characteristics of these bacteria, which in turn informs prevention and treatment strategies.
In everyday life, understanding the classification of Campylobacter can help individuals take targeted precautions to avoid infection. By being aware of the most common sources of transmission and taking steps to handle food safely, people can significantly reduce their risk of contracting this bacterial illness.
Common Sources of Infection
Campylobacter infections are often contracted through contaminated food and water sources. According to the World Health Organization (WHO), approximately 50% of campylobacter cases can be linked to poultry products, particularly chicken. It’s essential for consumers to handle raw chicken safely to prevent cross-contamination.
Chicken is not the only source of Campylobacter infection; other contaminated foods include beef, pork, and lamb. A study published in the Journal of Food Protection found that 1 in 5 meat samples from a grocery store contained Campylobacter bacteria. Fresh produce, such as lettuce and spinach, can also become contaminated through irrigation systems or poor handling practices.
To minimize the risk of infection, it’s crucial to follow proper food safety guidelines when preparing meals. Always wash your hands thoroughly before and after handling raw poultry. Separate cooked foods from raw foods to prevent cross-contamination, and store perishable items at a safe temperature below 40°F (4°C).
Avoid consuming untreated water from streams, lakes, or rivers, as these can harbor Campylobacter bacteria. Always use filtered or bottled water for drinking, cooking, and washing fruits and vegetables.
Symptoms and Diagnosis
If you suspect you have a campylobacter infection, it’s essential to understand its symptoms, which can be similar to other gastrointestinal issues. This section will guide you through the diagnostic process and common signs of illness.
Identifying the Signs of Infection
If you’re experiencing symptoms that could indicate a Campylobacter infection, it’s essential to be aware of the signs and seek medical attention if necessary. Gastrointestinal issues are common with this bacterial infection, often manifesting as diarrhea, abdominal pain, and cramping. The diarrhea may be watery or bloody, and the frequency can range from mild to severe.
Other symptoms associated with Campylobacter infections include fever, chills, nausea, and vomiting. In some cases, people may experience headaches, fatigue, and muscle aches. If you’re experiencing any of these symptoms after consuming undercooked poultry or other contaminated food items, it’s crucial to seek medical attention promptly.
To identify the signs of infection, look for a combination of gastrointestinal issues and fever. If your diarrhea is accompanied by blood or if you experience severe abdominal pain, seek immediate medical attention. Additionally, if you’re experiencing symptoms such as chills, nausea, or vomiting, don’t hesitate to consult with your healthcare provider for guidance on treatment and prevention.
It’s worth noting that some people may not exhibit any noticeable symptoms at all, while others may experience more severe complications, including Guillain-Barré syndrome in rare cases. If you suspect you’ve contracted a Campylobacter infection, follow the advice of your healthcare provider to ensure proper diagnosis and treatment.
Diagnostic Methods
Diagnosing Campylobacter infection can be a bit of a challenge, but fortunately, there are several methods that healthcare professionals use to identify the presence of this bacteria. The most common diagnostic method is through laboratory tests on stool samples.
When you visit your doctor with symptoms such as diarrhea, abdominal cramps, and fever, they will likely collect a stool sample from you for testing. This sample is then sent to a laboratory where it undergoes various tests to detect the presence of Campylobacter bacteria. These tests include:
* Culture: This involves growing the bacteria in a special medium to identify its characteristics.
* PCR (Polymerase Chain Reaction): A rapid test that detects specific genetic material from the bacteria.
* Immunological tests: These detect the antibodies produced by your body’s immune response to the infection.
Your doctor may also perform other diagnostic tests such as blood work or urinalysis to rule out other possible causes of your symptoms. If you suspect that you have a Campylobacter infection, it’s essential to seek medical attention promptly for proper diagnosis and treatment.
Risk Factors and Prevalence
To better understand the likelihood of contracting a campylobacter infection, let’s explore the common risk factors and prevalence rates worldwide.
High-Risk Groups
Young children and individuals with weakened immune systems are particularly susceptible to Campylobacter infections. In fact, studies have shown that people under the age of five are more likely to contract this bacteria due to their developing immune systems. For example, a study published in the Journal of Infectious Diseases found that infants and toddlers are at a higher risk of developing diarrhea-predominant Campylobacter infection.
Immunocompromised individuals, such as those with HIV/AIDS or undergoing chemotherapy, also face an increased risk of severe illness from Campylobacter. These individuals may experience more prolonged and severe symptoms, making it essential for them to take extra precautions when handling food and engaging in outdoor activities. To minimize the risk, caregivers should be vigilant about proper handwashing techniques, especially after changing diapers or interacting with pets that may carry the bacteria.
Additionally, pregnant women are also considered a high-risk group due to their weakened immune systems during this period. They should avoid consuming raw or undercooked poultry and eggs, which can contain Campylobacter. Regularly washing hands before handling food and cooking to an internal temperature of at least 165°F (74°C) can also help prevent the spread of infection.
Global Prevalence
Campylobacter infections are a widespread global health concern, with significant variations in incidence rates and geographic distribution. According to the World Health Organization (WHO), Campylobacter is one of the most common causes of diarrhea worldwide, accounting for an estimated 978 million cases annually.
In terms of incidence rates, Campylobacter infection affects approximately 1 in 100 people globally each year. This translates to a staggering 2.4% of the global population being infected with Campylobacter every year. The highest incidence rates are reported in low- and middle-income countries, where access to clean water, sanitation, and healthcare may be limited.
Geographically, Campylobacter infections are most prevalent in East Asia, Europe, and North America. However, even within these regions, there is significant variation in infection rates. For example, a study conducted in the United States found that the incidence of Campylobacter infection varied by state, with some states reporting rates as high as 20 cases per 100,000 people.
To put this into perspective, consider that for every reported case of Campylobacter infection, there are likely many more undiagnosed cases. This highlights the need for improved surveillance and diagnostic methods to better understand the true burden of Campylobacter infections globally.
Prevention and Control Measures
To minimize the risk of campylobacter infection, it’s essential to take proactive steps at home and when preparing food for others. We’ll explore effective prevention and control measures in this section.
Safe Food Handling Practices
When handling food to prevent Campylobacter infection, it’s essential to follow safe practices that minimize the risk of contamination. To start with, always wash your hands thoroughly before and after handling raw poultry, meat, and seafood. This includes under your nails, wrists, and between fingers.
It’s also crucial to store raw foods separately from cooked ones in sealed containers or zip-top bags to prevent cross-contamination. Raw meat, poultry, and seafood should be stored on the bottom shelf of the refrigerator, while ready-to-eat foods like fruits and vegetables go on higher shelves to prevent juices from dripping onto them.
When cooking, ensure that all poultry is cooked to an internal temperature of at least 165°F (74°C). Use a food thermometer to check for doneness, as this can be difficult to gauge visually. After cooking, let meat rest for a few minutes before serving to allow the juices to redistribute and reduce bacterial load.
Remember, proper handling, storage, and cooking techniques are your best defenses against Campylobacter infection. By following these simple guidelines, you’ll significantly reduce the risk of foodborne illness in yourself and others.
Personal Hygiene and Handwashing
When it comes to preventing the spread of Campylobacter infection, personal hygiene and handwashing play a crucial role. You see, this bacteria is often found on food and water, but it can also be carried on our hands and surfaces, making it easy to contaminate other areas and objects.
To put it into perspective, studies have shown that up to 40% of people with Campylobacter infection report no known risk factors, such as travel or contaminated food. This suggests that transmission through everyday contact is a significant concern.
So, what can you do? First, wash your hands frequently and thoroughly, especially after using the bathroom and before handling food. Use soap and water for at least 20 seconds to ensure you’re getting rid of any bacteria. Make sure to get between your fingers, under your nails, and the backs of your hands.
Also, avoid touching your face, particularly your mouth and eyes, as this can spread the bacteria easily. If you handle raw meat or poultry, make sure to wash your hands again afterwards.
By following these simple habits, you can significantly reduce your risk of getting Campylobacter infection through contact transmission.
Treatment and Management
Once you’ve been diagnosed with campylobacter, it’s essential to focus on managing your symptoms and preventing further complications through proper treatment. Here, we’ll outline the best practices for treating this bacterial infection.
Antibiotic Therapy
When it comes to treating Campylobacter infection, antibiotic therapy is often prescribed. However, not all cases of Campylobacter require antibiotics. In fact, the American Gastroenterological Association recommends against using antibiotics for uncomplicated cases of Campylobacter infection.
For those who do need antibiotics, the most commonly prescribed medications are ciprofloxacin and azithromycin. These antibiotics can help alleviate symptoms such as diarrhea and abdominal cramps. However, it’s essential to note that antibiotic use comes with risks, including increased risk of C. difficile infection, antibiotic resistance, and allergic reactions.
To minimize these risks, your doctor may prescribe a lower dose or a shorter course of treatment than usual. In addition, they may recommend probiotics to help restore the balance of good bacteria in your gut. It’s also crucial to complete the full course of antibiotics as directed, even if symptoms improve before finishing the medication.
When taking antibiotics for Campylobacter infection, be sure to drink plenty of fluids and electrolyte-rich beverages to stay hydrated. You should also avoid sharing food or utensils with others and wash your hands frequently to prevent the spread of the infection.
Alternative Treatments
When it comes to treating Campylobacter infection, some people may be looking for alternative approaches beyond conventional antibiotics. While these methods won’t replace medical treatment entirely, they can complement traditional care and support the body’s natural healing process.
Probiotics are one such alternative treatment that has gained attention in recent years. These beneficial bacteria can help restore the balance of gut flora, which is often disrupted by Campylobacter infection. Studies have shown that probiotics can reduce symptoms like diarrhea and abdominal pain, as well as enhance immune function. To incorporate probiotics into your treatment plan, choose a high-quality supplement containing strains specifically designed to target gastrointestinal health, such as Lactobacillus or Bifidobacterium.
Supportive care is another essential aspect of alternative treatment. This can include getting plenty of rest, staying hydrated with electrolyte-rich fluids like coconut water or sports drinks, and practicing stress-reducing techniques like meditation or deep breathing exercises. By supporting the body’s natural healing processes, you may be able to reduce recovery time and minimize the risk of complications.
In addition to probiotics and supportive care, some people find relief from herbal remedies like peppermint oil or slippery elm. However, it’s essential to consult with a healthcare professional before adding any new supplements or treatments to your regimen.
Complications and Long-Term Effects
While many people recover from a campylobacter infection without issue, some may experience complications that can arise days or even weeks after symptoms first appear. These complications can be serious and require medical attention.
Potential Complications
Campylobacter infection can lead to several potential complications that may require medical attention. One of the most serious and rare complications is Guillain-Barré syndrome (GBS), a autoimmune disorder where the body’s immune system attacks the nerves, causing muscle weakness and sometimes paralysis. According to the World Health Organization (WHO), GBS occurs in about 1 in 100,000 people who contract Campylobacter infection.
Other potential complications of Campylobacter infection include reactive arthritis, irritable bowel syndrome (IBS), and an increased risk of developing type 2 diabetes. In rare cases, the infection may also cause life-threatening conditions such as hemolytic-uremic syndrome (HUS) or thrombotic thrombocytopenic purpura (TTP).
If you suspect you have a Campylobacter infection, it’s essential to seek medical attention if you experience any of these symptoms: difficulty walking, weakness in the arms and legs, double vision, dizziness, or severe abdominal pain. Your healthcare provider may perform tests to determine the severity of your condition and provide treatment accordingly.
It’s also crucial to note that not all Campylobacter infections lead to complications, but if you’ve recently contracted the infection, monitoring your symptoms closely can help prevent potential complications.
Long-Term Effects on Health
If you’ve ever had a Campylobacter infection, you may be wondering if it has long-term effects on your health. Unfortunately, the answer is yes. Research has shown that people who have had Campylobacter infections are more likely to experience gastrointestinal issues down the line.
One of the most significant risks is irritable bowel syndrome (IBS). Studies have found that up to 50% of individuals with a history of Campylobacter infection go on to develop IBS. Symptoms can range from mild to severe and include abdominal pain, bloating, and changes in bowel movements. Even if you don’t experience full-blown IBS, you may still notice recurring digestive issues like diarrhea or constipation.
To minimize your risk of long-term health effects, it’s essential to take steps to manage stress and maintain a healthy gut microbiome. This can be achieved through diet, exercise, and relaxation techniques. Consider incorporating probiotics into your daily routine to support the growth of beneficial bacteria in your gut. Additionally, eating smaller, more frequent meals and avoiding trigger foods like gluten or dairy may help alleviate symptoms.
By being proactive about your health and taking steps to prevent long-term complications, you can reduce your risk of recurring gastrointestinal issues.
Frequently Asked Questions
What are the common mistakes people make when handling raw poultry to prevent campylobacter infection?
When handling raw poultry, it’s essential to avoid cross-contamination by washing your hands frequently, especially after touching raw meat, and keeping raw poultry separate from ready-to-eat foods. Additionally, always wash your hands with soap and warm water for at least 20 seconds before and after handling raw poultry.
Can I still get campylobacter infection if I thoroughly wash my fruits and vegetables?
Yes. While washing your fruits and vegetables can help reduce the risk of foodborne illness, it’s not a foolproof method to prevent campylobacter infection. Campylobacter can be present on produce that has been contaminated with animal feces during growth or harvesting.
How long does it typically take for symptoms of campylobacter infection to appear after exposure?
Symptoms of campylobacter infection usually appear within 2-5 days after exposure, but they can occur as soon as one day or up to a week later. The incubation period can vary depending on several factors, including the severity of the infection and individual immune response.
Are people who have had previous campylobacter infections more likely to experience long-term effects?
No. While some individuals may experience lingering gastrointestinal symptoms or fatigue after recovering from a campylobacter infection, there is no conclusive evidence that people with prior infections are at higher risk for developing long-term complications. However, it’s essential to consult a healthcare professional if you’re experiencing persistent or severe symptoms.
Can I safely eat undercooked meat during the winter months when foodborne illnesses are less prevalent?
No. Campylobacter can be present in raw poultry and meat throughout the year, regardless of the season. Undercooking or consuming raw meat increases your risk of contracting campylobacter infection, even during winter months. Always cook meat to an internal temperature of at least 165°F (74°C) to ensure food safety.
